Summary
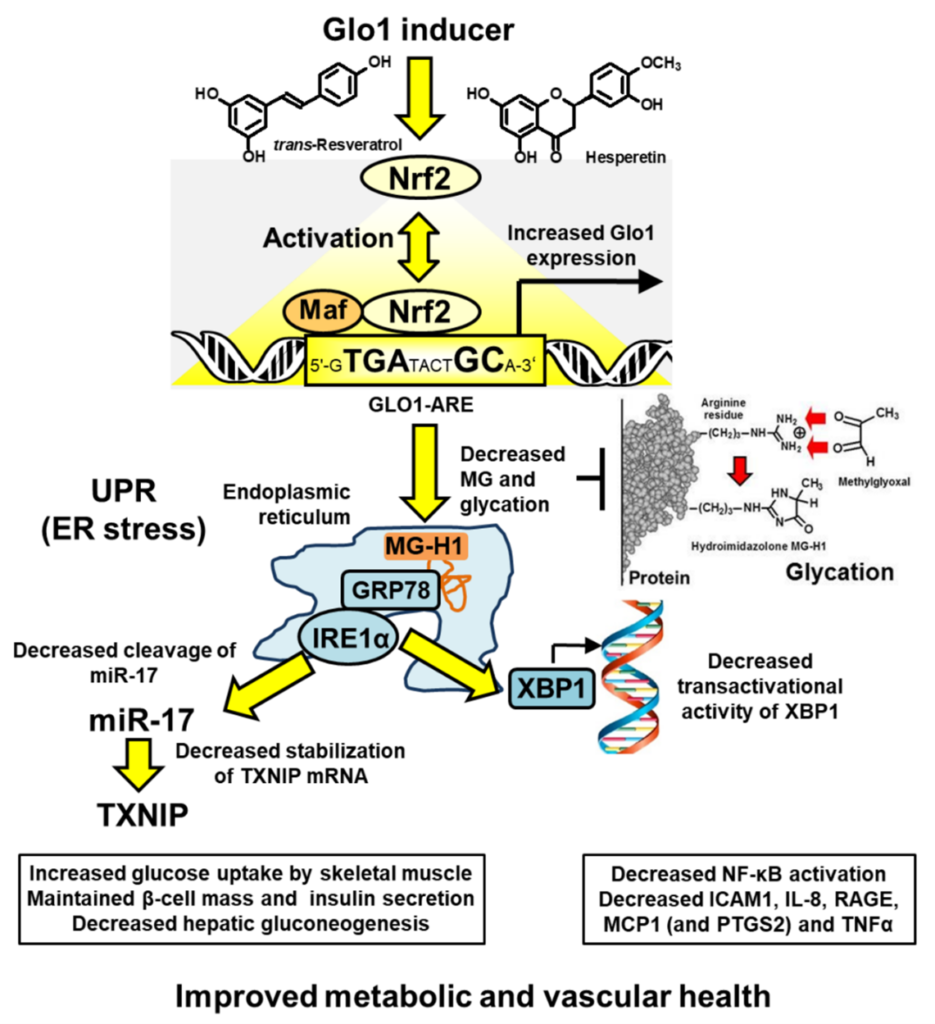
The abnormal accumulation of methylglyoxal (MG) leading to increased glycation of protein and DNA has emerged as an important metabolic stress, dicarbonyl stress, linked to aging and disease. Increased MG glycation produces inactivation and misfolding of proteins, cell dysfunction, activation of the unfolded protein response and related low grade inflammation. Glyoxalase 1 (Glo1) of the glyoxalase system has a major role in the metabolism of MG. Small molecule inducers of Glo1, Glo1 inducers, have been developed to alleviate dicarbonyl stress as a prospective treatment for the prevention and early-stage reversal of type 2 diabetes and prevention of vascular complications of diabetes. The first clinical trial with the Glo1 inducer, trans-resveratrol and hesperetin combination (tRES-HESP) – a randomized, double-blind, placebo-controlled crossover phase 2A study for correction of insulin resistance in overweight and obese subjects, was completed successfully. tRES-HESP corrected insulin resistance, improved dysglycemia and low grade inflammation. These findings suggest tRES-HESP counters MG accumulation and protein glycation, decreasing activation of the unfolded protein response and expression of TXNIP and TNFα, producing reversal of insulin resistance. tRES-HESP is suitable for treatment of insulin resistance and related disorders.
Summary scheme
Principal publications
Rabbani, N. and Thornalley, P.J. (2022) Emerging glycation-based therapeutics – glyoxalase 1 inducers and glyoxalase 1 inhibitors. Internat J. Molec. Sci. 23, 2453.
Further information at https://glocentrica.com/glyoxalase-1-inducer/
Thiamine deficiency in diabetic patients – Role of thiamine therapy for prevention and treatment of early-stage diabetic nephropathy
Diabetes is associated with multiple pathways of biochemical dysfunction (Fig1) linked to the development of vascular complications. We proposed a strategy to counter biochemical dysfunction linked to the development of vascular complications is high-dose therapy with thiamine and related derivatives such as benfotiamine. High-dose thiamine therapy prevented the development of microvascular complications in experimental diabetes without improvement of metabolic control. Experimental diabetes was also associated with tissue specific thiamine deficiency characterised by a marked decrease of plasma thiamine concentration and decreased activity of the thiamine-dependent enzyme of transketolase (TK) and decreased levels of TK protein in renal glomeruli linked to a profound increase in renal clearance of thiamine (ClThiamine) [1]. Thiamine deficiency was not detected by the conventional indicator of thiamine status, the erythrocyte ‘thiamine effect’ (the percentage unsaturation of TK with thiamine pyrophosphate [TPP] cofactor). We found prevalence of similar low plasma thiamine concentrations and impaired renal handling of thiamine in clinical diabetes (2). We conducted a pilot study, and evaluated the effect of oral high dose supplements of thiamine on urinary albumin excretion (UAE), a marker of early-stage diabetic nephropathy, in type 2 diabetic patients with microalbuminuria. Clinical trial was funded by Pakistan Higher education Commission and conducted in Pakistan [3].Fig 1. Multiple pathways of biochemical dysfunction linked to the development of vascular complications. Thiamine supplementation counters metabolic dysfunction linked to microvascular complications of diabetes.

Fig 2. The time course of changes in Urinary Albumin Eexcretion (UAE) in patients treated with thiamine and placebo showed progressive decrease in UAE with time through out the treatment period. Linear regression of UAE in relation to treatment time indicated that the rate of decrease in UAE was increased about 4 fold in patients treated with thiamine compared to placebo.
